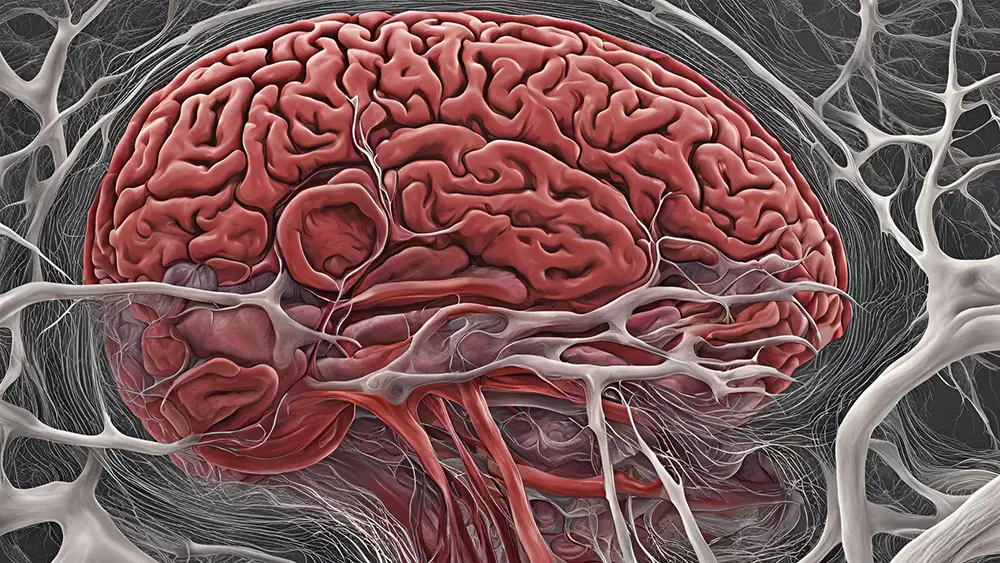
Imagine your brain as a highly fortified fortress, guarding the most precious command center of your body. This impenetrable barrier, known as the blood-brain barrier (BBB), stands as a vigilant gatekeeper. It meticulously controls the flow of molecules between the bloodstream and the delicate neural tissue. It’s a marvel of biological engineering, and understanding its intricacies is crucial for anyone pursuing a career in the scientific realm.
So, what exactly is this blood-brain barrier?
It’s a highly selective, semi-permeable membrane that shields the brain from potentially harmful molecules. It does this while allowing essential nutrients and compounds to pass through. Acting as a biological firewall, the BBB protects the brain’s vulnerable microenvironment, maintaining a homeostatic balance that enables optimal neuronal function.
The BBB is essential because the brain is a sensitive organ. Even slight disruptions in its chemical composition can have catastrophic consequences. By carefully regulating the flow of molecules, the BBB safeguards the brain from toxins, pathogens, and fluctuations in blood composition that could compromise its delicate operations.
Unraveling the precise functions and interactions of each cell type is fundamental to understanding how the neurovascular unit operates. It could reveal new insights into BBB biology. In turn, this has implications for drug delivery and neurological disease.
So, what are the different cells in the blood-brain barrier?
What is the Blood-Brain Barrier?
The blood-brain barrier is a complicated labyrinth of cells in the brain. These cells form a protective layer that lines the inside of the brain’s blood vessels.
It’s important to know that the term “barrier” is a bit of a misnomer. The BBB acts more like a filter or a gatekeeper for your brain.
The purpose of the BBB is to keep potentially harmful molecules out and keep helpful ones inside. The cells control how various chemicals and molecules enter and exit your brain.
Cells in the Blood-Brain Barrier
The blood-brain barrier is mainly composed of several cell types including:
- Capillary endothelial cells
- Astrocytes
- Pericytes
- Vascular Leptomeningeal Cells
- Neurons
- Basement membrane
- Microglia

All these cells contribute to immunological function. Together, they are often called a neurovascular unit, or NVU. They preserve a healthy BBB to guarantee a healthy brain and appropriate central nervous system activities.
Endothelial Cells
Endothelial cells come from the mesodermal germ layer. They are a type of simple squamous epithelial cell. Endothelial cells line the inside walls of delicate blood vessels called capillaries.
The endothelial cells in the brain are different. They have some unique features compared to those in other parts of the body. For example, brain endothelial cells experience polarization. This means they have distinct inner and outer surfaces.
Brain endothelial cells form tight junctions between each other. Think of it like very snug zippers sealing the cells together. They also have junctional adhesion molecules that help bind the cells. Brain endothelial cells have specialized transport systems. Such systems control what polar (charged) substances can cross the cell barrier.
These cells contain many mitochondria. They are the powerhouses producing ATP energy for the cell. The mitochondria also help regulate the ion gradients needed for transport functions across the cell membrane. It’s thought that brain endothelial cells have a distinct metabolism that alters substances’ physical properties like solubility to create a protective barrier.
Two nearby cell types influence the brain endothelial cells: pericytes and astrocytes. More specifically, the endfeet processes affect the endothelial cells. Proteins on their surfaces enable signaling between these cells. Signaling also occurs because of connections to internal scaffolding proteins like:
- Zonula occludens
- Actin cytoskeleton
- G-proteins
- Protein kinases
The endothelial cells use very tight junctional complexes to seal themselves together. These are much tighter than junctions in ordinary capillaries elsewhere. The tightness of these junctions severely restricts passive molecule movement across the cells into the brain. It gives brain blood vessels extremely high electrical resistance across the endothelial layer.
Claudin and occludin proteins form the tight connections that connect to the actin cytoskeleton inside via zonula occludens scaffolds. Claudin-3, -5, and -12 are key for this high resistance barrier. If these proteins’ regulation goes awry, it can compromise the blood-brain barrier. In turn, this could allow toxins to enter the brain environment.
Astrocytes
Astrocytes are star-shaped cells that are very abundant. They have many important roles in the brain and nervous system.
Astrocytes guide the migration of developing neurons during brain growth. They also act as buffers, helping to regulate potassium ion levels. These cells are also capable of removing excess neurotransmitter molecules.
Astrocytes have a distinctive stellar shape with several branch-like processes extending out. One of their defining characteristics is the ability to produce two types of structural proteins:
- Vimentin
- Glial fibrillary acidic protein
A notable feature of astrocytes is their endfeet processes. They cover essentially the entire surface area of blood vessels in the brain.
Astrocytes develop from radial glia and neural precursor cells later in pregnancy. However, they don’t control the initial formation of the blood-brain barrier.
The astrocyte endfeet that surround brain capillaries have potassium channels. These channels are critical for regulating:
- Water balance
- Ionic concentrations
- Proper blood-brain barrier function
Many studies suggest astrocyte activities are essential for a fully functional blood-brain barrier. It is also essential for promoting repair if it gets disrupted after brain injury.
During inflammation, astrocytes can shift into two phenotypes called A1 and A2. Gene studies show the A1 form is harmful with increased levels of complement proteins. The A2 phenotype has more healing properties. Lack of astrocyte interaction with brain blood vessels could disrupt the integrity of the blood-brain barrier in multiple sclerosis models.
Pericytes
Pericytes are cells located in between endothelial cells, astrocytes, and neurons. Endothelial cells form the walls of capillaries in the brain. Pericytes have an important job. They interact and connect with the endothelial cells of the blood-brain barrier.
Pericytes and endothelial cells need to communicate well. This communication allows the proper formation, growth, stability, and maintenance of the functional blood-brain barrier. Pericytes help control how permeable the blood-brain barrier is. Pericytes also regulate the blood flow in the brain.
Pericytes can engulf and clear away harmful foreign substances. This process is called phagocytosis. If pericytes become dysfunctional or are missing, it can really disrupt the blood-brain barrier. Abnormal pericytes likely contribute to the disease processes of many illnesses. These illnesses involve instability of the brain’s small blood vessels and blood-brain barrier.
Microglia
Microglia are a type of glial cell. Glial cells are found in the nervous system. Microglia are distributed throughout the brain and spinal cord. In brain tissue, microglia make up around 5-20% of all glial cells.
Microglia have important jobs that support nerve cells. One job is providing immune defenses. Microglia engulf and remove dangerous foreign particles. Another job is helping to repair injured areas of brain tissue. Microglia also participate in signaling between cells outside of cells.
There is more and more evidence about activated microglia. Activated microglia can regulate the expression of tight junction proteins. When this happens, it improves the integrity and function of the blood-brain barrier.
The specialized characteristics of the blood-brain barrier are maintained by many cells working together. This includes microglia and other components that make up the neurovascular unit. The interactions between these cells are ongoing and dynamic. These interactions control the barrier.
Vascular Leptomeningeal Cells
When it comes to the cellular team players that make up the blood-brain barrier, one group doesn’t get as much time in the spotlight – the vascular leptomeningeal cells (VLMCs). But make no mistake, these underrated cells are crucial members of the brain’s security force.
So, what exactly are VLMCs?
They are cells that form the leptomeninges. Leptomeninges are the two innermost membranes that envelop and protect the brain and spinal cord. Essentially, they keep the delicate neural tissues safe and secure.
VLMCs play a role in maintaining the brain’s internal environment too. They have intimate physical associations with the blood vessels in the subarachnoid space between the meningeal layers. That makes this type of cell critical auxiliary gatekeepers work alongside endothelial cells.
VLMCs use their elongated processes to wrap around and stabilize the brain’s microvessels. This physical coverage creates a secondary barrier. This second barrier regulates molecular movement in and out of the cerebrospinal fluid.
Researchers think VLMCs have some involvement in clearing waste products from the CNS interstitial fluid into the bloodstream. They are also thought to modulate:
- cerebral blood flow
- immune responses when required
Basement Membrane
The basement membrane is an important part of the blood-brain barrier. It is not just cells and biomolecules that are involved. The basement membrane helps regulate the permeability of the barrier. It connects cells together. It also helps cells communicate with each other. The basement membrane interacts with proteins outside of cells to control the barrier function.
The basement membrane is made up of many different molecules. These include collagen, nidogen, laminin, sulfated molecules, proteoglycans, and other glycoproteins. The endothelial cells that form capillary walls have receptors called integrins. The integrins are alpha and beta types. The integrins allow the endothelial cells to bind to proteins in the basement membrane. These proteins include collagen, perlecan, and laminin.
The basement membrane acts as an anchor for signaling events in blood vessels. But it also prevents chemicals and cells from passing into the brain tissue. It acts as a barrier. Sometimes the basement membrane gets disrupted by enzymes called matrix metalloproteinases. When this happens, it impairs the function of the blood-brain barrier. It allows inflammatory cells called leukocytes to leak into the brain. This leakage is seen in various neurological diseases.
Where the Blood-Brain Barrier is not…
The blood-brain barrier (BBB) is a protective barrier that controls the movement of molecules between the blood and the brain’s extracellular fluid. However, there are certain areas in the brain called circumventricular organs (CVOs) where the BBB is either missing or very permeable.
The CVOs are located around the third and fourth ventricles of the brain and include the following structures:
- Pineal gland
- Median eminence
- Subcommissural organ
- Neurohypophysis
- Subfornical organ
- Area postrema
- Organum vasculosum of the lamina terminalis
Unlike the rest of the brain, the blood vessels in the CVOs have openings that allow molecules to pass through easily. This is important for their function.
CVOs help regulate different automatic and hormonal functions in the body. By letting molecules move freely between the blood and the brain, the CVOs can detect and respond to changes in hormone levels, nutrients, and other signals in the blood.
This feature allows the CVOs to act as communication centers, sending information about the body’s internal conditions to the brain. This helps coordinate responses through the autonomic nervous system and endocrine glands.
While the BBB is essential for protecting the brain from harmful substances, the absence of this barrier in the CVOs allows for important processes like regulating fluid balance, blood pressure, and hormone release, ensuring the body functions properly.
Conclusion
The blood-brain barrier is an amazing system made up of different types of cells that protect the brain while letting important nutrients and signals pass through. This system works well because of the coordination between several specialized cell types.
Endothelial cells form the main barrier, sealing the blood vessels tightly. They get crucial help from nearby pericytes and astrocytes. Pericytes help control blood flow and remove toxins, while astrocytic endfeet help keep the balance of ions.
Even less noticed parts, like the basement membrane and extracellular matrix, are important. They provide structural support and help the different cells communicate to control the barrier’s permeability.
The neurovascular unit and blood-brain barrier show how complex the body is, with individual cells working together like a team to protect the brain.
Delivering treatments past this barrier is challenging, but research is making progress. Understanding how these cells and molecules interact could lead to new methods, like using nanoparticles or safely adjusting the barrier temporarily.
So, when you think about the amazing capabilities of the human brain, remember the hard-working cells of the blood-brain barrier. Without these protective cells, the brain’s genius wouldn’t be possible.